Large Intestines
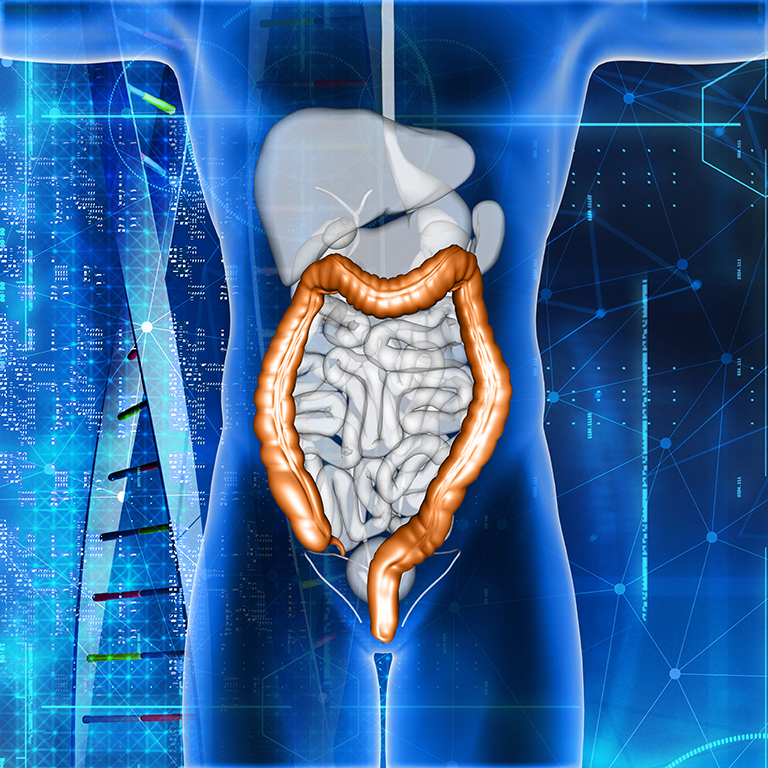
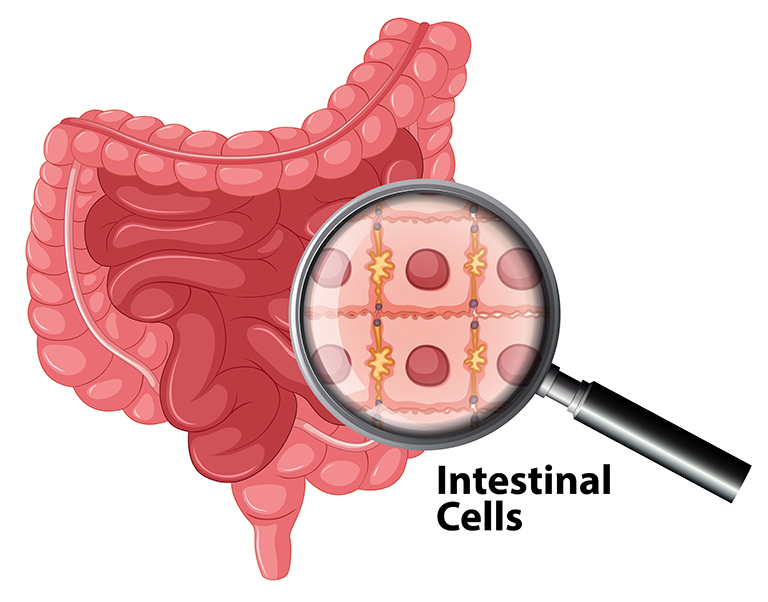
The colon is part of the digestive system. The digestive system separates vitamins, minerals, carbohydrates, fats, proteins and water from the nutrients taken and ensures the removal of waste materials from the body. The digestive system consists of the esophagus, stomach, small intestines, and large intestines. The first part of the large intestine is called the colon, and the last part, together with the rectum, forms the anal canal. The average length of all large intestines is 150 cm, and the last 15 cm of this is the anal canal and rectum.
The large intestine consists of five main parts;
- First part; Ascending colon (right colon); It starts with the part called the cecum where the small intestines meet and extends upwards to the right of the abdomen.
- Second part; Transverse colon; extends horizontally from right to left in the upper part of the abdomen.
- Third part; Descending colon (descending - left colon); extends from the left side of the abdomen from top to bottom.
- Fourth part; sigmoid colon; It is given this name because it is in the "S" or sigmoid shape.
- Fifth part; Rectum; The material consisting of waste materials passes through the large intestines and reaches the rectum. This is called feces (feces-stool). Stool is stored in the rectum and then expelled from the body through the anus.
COLON (COLO-RECTAL) CANCER

Colon cancer is cancer of the large intestine. The last part of the digestive system is called the rectum, and the rectum is actually the name given to the last part of the colon. However, colon cancers are generally referred to as colorectal cancers. More than 95% of colorectal cancers are adenocarcinomas. To a lesser extent; carcinoid tumors, gastrointestinal stromal tumors (GIST), lymphoma, sarcoma can be seen.
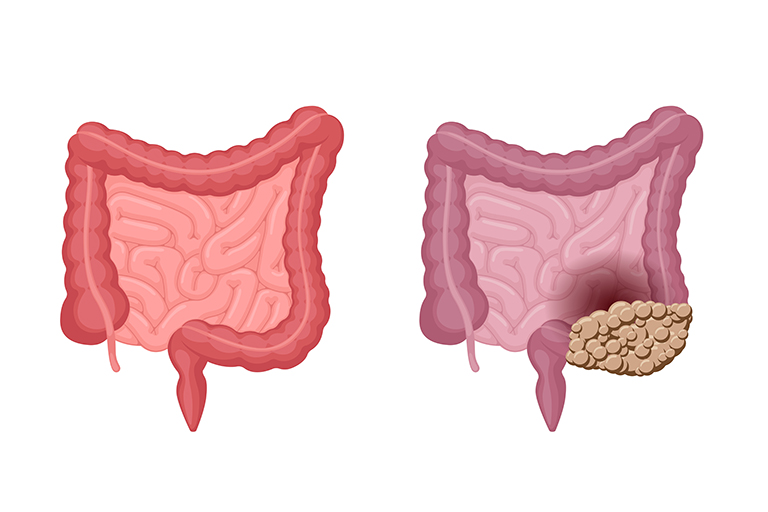
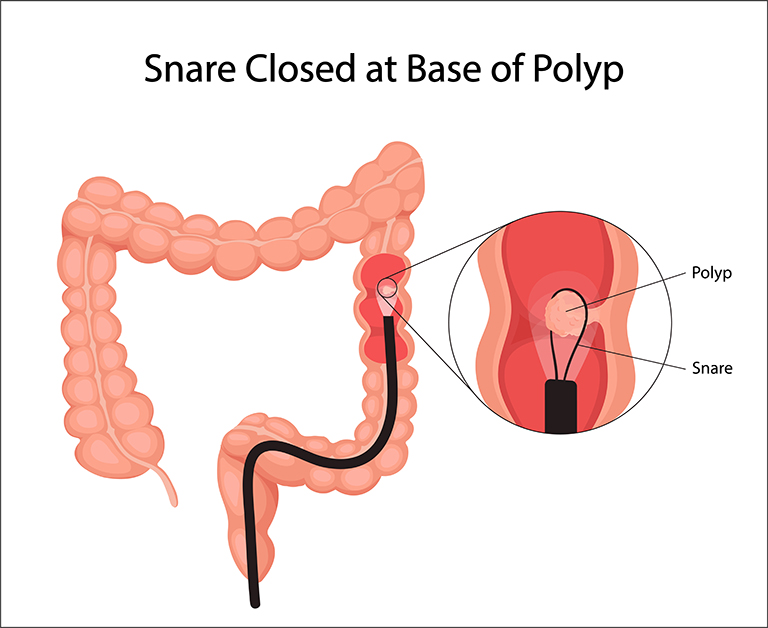
Most colon cancers initially develop from a benign (benign) piece of tissue called an adenomatous polyp. Some of these benign polyps turn into colon cancer over time.
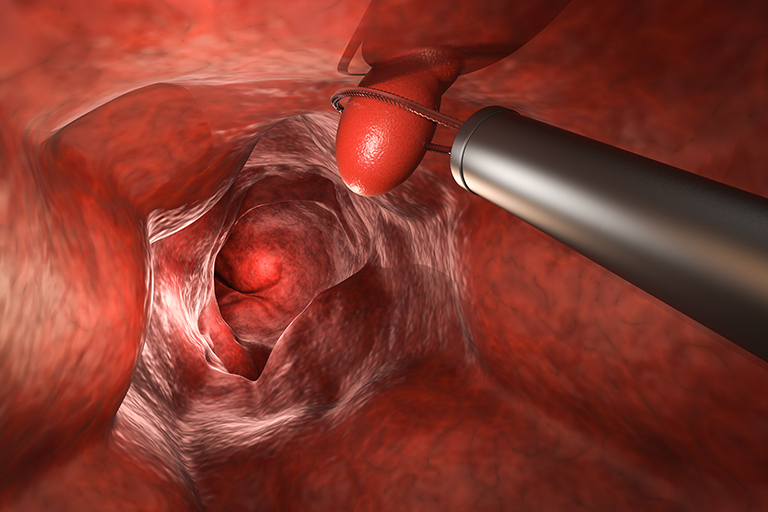
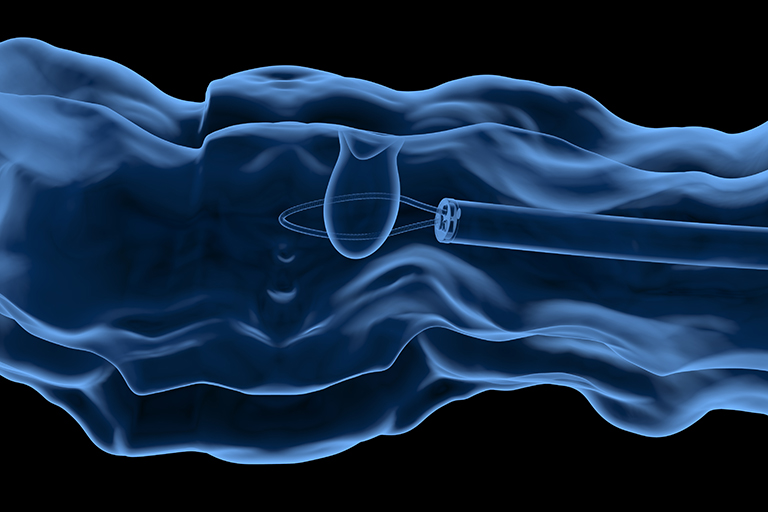
Polyps are small lesions that usually do not cause any complaints. Therefore, regular controls are of great importance in the prevention of colon cancer. When these polyps are removed with a timely colonoscopy, they are prevented from turning into cancer in the future.
WHAT ARE THE CAUSES OF COLORECTAL CANCER DEVELOPMENT?
- In most patients, the exact cause is not clear.
- Precancerous (tumor development potential) lesions; The vast majority of colon cancers originate from polyps arising from the intestinal wall. Early removal of polyps when they are detected prevents the development of cancer.
- Some inherited gene mutations
- Familial adenomatous polyp (FAP); There are thousands of polyps in the colon and rectum, and these patients usually develop cancer before the age of 40.
- Hereditary nonpolyposis colorectal cancer (HNPCC); Also called Lynch syndrome. Colon and other types of cancer can also develop, often before the age of 50.
WHAT ARE THE RISK FACTORS IN COLORECTAL CANCERS?
Factors that increase your chance of getting the disease are called risk factors;
- Advanced age; 90% of diagnosed patients are over 50 years of age
- Having had colorectal cancer, ovarian, endometrial or breast cancer in the past
- People who have had previous interventions for colorectal polyps
- Inflammatory bowel diseases; having diseases such as ulcerative colitis, Crohn's disease
- Certain hereditary conditions; genetic diseases such as familial adenomatous polyposis (FAP), hereditary nonpolyposis colorectal cancer (HNPCC; Lynch syndrome)
- Presence of a family history of colon cancer or colon polyps
- A diet rich in low fiber and high fat and red meat
- Sedentary lifestyle; sedentary and physical activity lifestyle
- Diabetes
- Being overweight (Obesity)
- Cigarette smoking
- Excessive alcohol use
- To have received radiation (radiation therapy) treatment; Having received abdominal radiotherapy for a pre-existing cancer may increase the risk of colon cancer.
FINDINGS AND SYMPTOMS IN COLORECTAL CANCERS
- Change in bowel habits (periodic constipation or diarrhea)
- Presence of blood in the stool (may be red or black in color)
- The stool is thinner than before
- Complaints such as cramps, gas and pain in the abdomen
- Feeling of incomplete emptying of the intestines after defecation
- Weakness or fatigue
- Unexplained weight loss
Most patients with colon cancer do not show symptoms in the early stage of the disease. The onset of symptoms is usually related to the size and location of the cancer.
DIAGNOSIS
- Physical examination and taking the patient's history
- Rectal digital examination; examining the presence of a palpable mass or fullness by finger examination from the anus
- Occult blood in stool; investigating whether there is blood in the stool by looking with a microscope
- Barium graphy; Controlling the intestines with X-rays after giving the liquid containing barium from the rectum. Today, it has been replaced by computed tomography taken after oral contrast drug administration.
- Sigmoidoscopy; The inside of the rectum and sigmoid colon is viewed with a thin, flexible finger-thick device with a video camera system at the end. When a polyp, suspicious area or cancer is seen, a biopsy can be taken from there and examined under a microscope.
- Colonoscopy; The entire large intestine is examined with a thin, flexible finger-thick device with a video camera system at the end. When a polyp, suspicious area or cancer is seen, a biopsy can be taken from there and examined under a microscope.
- DNA test in stool; In a stool sample, the presence of abnormal DNA seen in polyps and cancers is investigated.
- Computed tomography colonography (Virtual colonoscopy); creation of three-dimensional images of the colon and rectum from the images obtained by computed tomography.
What are the factors that are affecting in determining the prognosis and the treatment option?
- Stage of cancer
- Whether the cancer completely occludes the large intestine
- Whether cancer cells remain after surgery
- If the cancer has recurred
- General health status and conditions of the patient
STAGING
Stage I: Cancer is limited to the superficial layer lining the inner surface of the colon or rectum (mucosa), the presence of cancer that has not extended beyond the intestinal wall.
Stage II: The cancer has invaded the rectum or colon wall but has not spread to nearby lymph nodes.
Stage III: Cancer has spread to surrounding lymph nodes but has not spread to other parts of the body
Stage IV: Cancer has spread (metastasized) to distant organs such as liver and lungs
WHAT ARE THE TREATMENT METHODS IN COLORECTAL CANCERS?

- Treatment in early-stage colorectal cancer;
If the cancer is small and limited to a polyp, the entire cancer can be removed with a polypectomy (removal of the polyp) performed during colonoscopy and no surgery is required. Larger polyps can be completely removed with the endoscopic mucosal resection method, again without the need for surgery. In both cases, in order to avoid the need for surgery, pathological examination should confirm that the tumor is completely removed, and no cancer tissue is left behind. - In the presence of polyps or cancer that cannot be removed by colonoscopy, colorectal surgery can be performed laparoscopically or robotically;
Removal of the diseased part of the large intestine or rectum with instruments inserted through finger-thick incisions (1-2 cm) small enough for the video camera system and other thin hand tools to enter. - Treatment in invasive colorectal cancer;
If the entire intestinal wall is advanced enough to not allow removal by colonoscopy, or if it has progressed to the surrounding tissues, the cancerous large intestine is surgically removed (partial colectomy). Neighboring lymph nodes are also removed in the same order and the intact intestinal ends are stitched together to make an anastomosis. Sometimes, after the cancerous part of the intestine is removed, the exposed parts of the intestine cannot be stitched together, in this case the exposed part of the intestine is mouthed to the skin (colostomy). A special bag (colostomy bag) is attached to the place where the intestine meets the skin and this bag is changed or emptied as it fills. Depending on the type of surgery performed and the stage of the disease, colostomies can be opened permanently or temporarily to be closed after recovery. - Surgery in advanced colorectal cancers;
In the presence of advanced cancer or if the general condition of the patient is too bad to withstand a heavy surgery, a colostomy is opened above the occluded place in order to eliminate the complaints related to intestinal obstruction (such as pain, inability to defecate, gas, nausea, vomiting) caused by the cancer. In emergencies due to bleeding, limited surgery involving the cancerous tissue can be performed.
In some special cases, for example, in cases where the cancer has spread to the liver along with colorectal cancer, both the cancerous part of the intestine and the cancerous parts of the liver can be removed together in the same session or separately by surgery to be performed in two different sessions. Sometimes, this surgery can be performed after chemotherapy is applied before the cancerous tissues are expected to shrink or to reach an operable number and size.
CHEMOTHERAPY

Chemotherapy is drug therapy applied to destroy cancer cells. In colorectal cancers, it is often given after surgery if tumor size is big or cancerous cells are found in the lymph nodes according to the pathology report. The aim is to minimize the chance of cancer recurrence (recurrence).
It is also used in patients with spread to other organs of the body. It is used to reduce the complaints or in cases where the cancer is too large to be removed or where there is a large number of cancer spread (for example, the liver) to reduce the tumor tissues to sizes that can be removed by surgery.
In rectal cancer, chemotherapy is used together with radiotherapy.
RADIOTHERAPY

High energy sources such as radiotherapy X-ray; It is applied to destroy cancer cells that are likely to remain after the surgery, to shrink the large tumor so that it can be easily removed in surgery, or to reduce complaints related to colorectal cancer.
It is rarely used in early stage colon cancer, but it is applied in every patient in rectal cancer, especially if the cancer has completely invaded the rectal wall and spread to neighboring lymph nodes. It is often used in conjunction with chemotherapy. It can be applied after surgery in rectal cancer to reduce the risk of cancer recurrence.
PREVENTION FROM COLORECTAL CANCER

Normal ordinary people should be checked for the development of colorectal cancer after the age of 50. In people with a family history of colon cancer or other risk factors, controls should start at an earlier age.
- Change in lifestyle
- A diet rich in fruits, vegetables and whole grains. These foods are rich in vitamins, minerals, fibers and antioxidants and may be beneficial in cancer prevention.
- Avoiding excessive alcohol intake, avoiding drinking if possible
- Stop smoking
- Exercising frequently
- Exercising for at least 30 minutes a day, if possible
- Maintaining your normal weight, avoiding excess weight
We can reduce the risk of colon cancer by making some changes in daily life.
- Colon cancer prevention in high-risk individuals
- Aspirin; Although some studies show that regular aspirin intake reduces the possibility of polyps and cancer development, it should not be forgotten that aspirin use can cause ulcers and bleeding in the digestive system.
- COX-2 inhibitors; Although there are some scientific studies that reduce the risk of developing precancerous (possible to turn into cancer) polyps, it is necessary to keep in mind the risk of developing heart disease with these drugs.
- Surgery to prevent cancer; In some rare hereditary diseases such as familial adenomatous polyposis (FAP) or inflammatory bowel diseases such as ulcerative colitis, the entire large intestine and rectum can be surgically removed to prevent cancer development on this ground.
Although there are studies showing that some drugs and surgeries reduce the risk of colorectal cancer in high-risk individuals, we do not have enough data to support their definitive application.
